The Sitting Sickness
If you've heard that life is movement, it's true. If you've heard that just sitting around can kill you, it's also true. Physical inactivity is the fourth leading cause of death worldwide! You may have heard the media reporting recently on several studies showing that prolonged sitting significantly increases the risk for death, including death from heart disease and cancer, but I'm not sure this news has really hit home yet.
Most people know that exercise is critical for health and preventing disease, but the issue of physical activity and inactivity is much bigger than exercise. Regardless of the amount of exercise one performs, the level of aerobic fitness one exhibits, or whether a person is thin or overweight, stillness still kills. Apparent health and leading an otherwise healthy lifestyle does not compensate for extended periods of sitting around, and we Americans do a great deal of sitting around.. We've even built over 4 million miles of roads so we can sit still while we go places! In fact, the infrastructures and cultures of most developed nations seem to be perfectly designed for physical inactivity.
The average American watches around 40 hours of television per week, while those over 65 watch an average of 48 hours per week. I've already written about the harms of television, computer, and tablet use as well as the related media consumed through these devices on GreenMedInfo (see "
Do You Have Facebook Affective Disorder"). Sitting is certainly one factor that contributes to the negative health consequences of these technologies. But there is another gigantic part of modern life in which sitting is the dominant physical activity (or inactivity!). I'm talking about work! The average American spends 40 hours per week watching television, 50 hours per week sleeping, and about 45 hours working (unless unemployed/retired). That leaves about 33 hours per week for other things, many of which also involve sitting (eating, checking Facebook and email, texting, driving/traveling... sometimes all together, but that is a different newsletter).
Many people, of course, work longer hours and, while some types of work are physically intense, "sitting jobs" are common. One study showed that office workers spend 95% of their time at work sitting and 82% of this time was nearly motionless! For many people, then, work contributes 45 hours of or so of physical inactivity per week embedded within 168 hours of mostly physical inactivity per week! Yet, work can also be 45 hours or so of physical activity per week if one chooses! While it is obvious that television viewing and other sedentary leisure activities can easily be replaced by more physically active leisure pursuits, we have overlooked the workplace as an additional source of potential physical activity!
This is a rather recent realization, and you may have observed, in response, the growing trend of treadmill desks and stand up desks. However, it is not that simple. Standing, per se, is not really the answer and we don't all need treadmill desks either. In this article, I want to explore the fascinating physiology of physical inactivity and muscle endocrinology a bit, and then focus in on the key to avoiding the harms of physical inactivity. Throughout the article, I'll use the term "low-amplitude low-intensity movement". This term refers to very small movements with minimal to no displacement of the body (low-amplitude) and which produce minimal to no sense of effort (low intensity). The bottom line is, physical activity in the form of low-amplitude low-intensity movement is critical for health and no supplement regimen, dietary modification, or exercise plan can compensate for its lack! It is time that we stand up to our sitting culture and demand opportunities to move!
The Many Faces of Sitting:
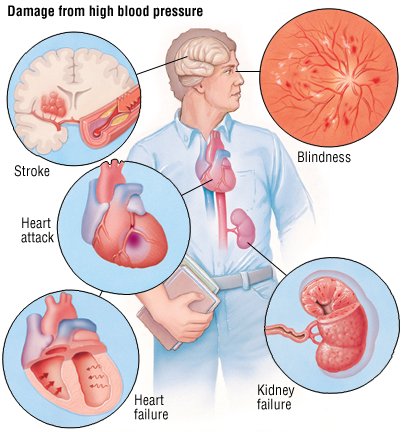
The data is solid; prolonged sitting is unhealthy and it doesn't matter so much whether that stillness is in front of a television or a desk, at home or work, or in a car or airplane. Not surprisingly, the harmful consequences of prolonged sitting are numerous. Studies have shown that prolonged sitting shortens life expectancy, increases fat accumulation around the heart, and is associated with metabolic syndrome (abnormal cholesterol or triglycerides, high blood pressure, insulin resistance, and abdominal obesity).
In an excellent article from 2009, Bente Petersen describes what he calls the "diseasome of physical inactivity". He says, "the diseasome of physical inactivity [is] mediated through an interdependent cycle of myokine imbalance or deficiency, immuno-endocrine dysfunction, and abdominal obesity". His argument needs little additional justification as it is thoroughly supported by modern physiology. The physical and physiological derangements which underlie Petersen's diseasome of physical inactivity include abdominal obesity, chronic inflammation, insulin resistance, atherosclerosis, neurodegeneration, and tumor growth. The resulting cluster of diseases includes type 2 diabetes, cardiovascular disease, depression, dementia, colon cancer, and breast cancer. These relationships are illustrated in "figure 1" below. Remember, by physical inactivity, we are not just referring to a lack of exercise. Instead, we are referring to prolonged periods of sitting still, regardless of how much exercise is done.

Figure 1: The Diseasome of Physical Inactivity
The Myokines, Mitochondria, and Metabolic Hormones of Movement:
With every new day, we glimpse the complexity of the human body a bit more, and we laugh (or cry) at the embarrassingly simple assumptions we held in the past. This is certainly true for muscle physiology. It was once thought that skeletal muscle cells were just the energy-using, mechanical end-organ of movement. Yet, today, we realize that skeletal muscle has the capacity to express several hormones and chemical messengers which influence a number of other tissues in the body (probably ALL of the tissues in the body). Scientists are calling these muscle messengers "myokines" and they are critical to explaining the "diseasome of physical inactivity." It appears that this "diseasome" results from a myokine deficiency! The list of known myokines includes lipoprotein lipase, interleukin (IL)-6, IL-8, IL-15, brain-derived neurotrophic factor (BDNF), leukemia inhibitory factor (LIF), fibroblast growth factor 21 (FGF21), and follistatin-like-1. I know, the scientific jargon is beautiful and exciting! What is more exciting, though, is that most of these myokines are released as a result of muscle contraction. Simply by contracting a muscle, one can get a micro-boost of disease preventing myokines! This is a rather radical realization, as it points out that a part of our endocrine system is directly under conscious control! So, let us explore a few myokines briefly so that we might better appreciate the endocrine effects of movement and muscle contraction on our bodies.
Lipoprotein Lipase: Lipoprotein lipase (LPL) is critical for the cellular uptake of triglycerides and the production of "good" HDL-cholesterol. Scientists have long searched for a drug to increase LPL activity in order to treat high triglycerides, cholesterol disorders, and cardiovascular disease. Well, it turns out that a scientific breakthrough is not needed at all, just some muscle contraction. Studies have shown that specific gene mutations that reduce LPL function or production are associated with a 5-fold increase in the odds for heart disease and death. This gene mutation can essentially be mimicked by inactivity. If the muscles do not contract, LPL production is minimized. On the other hand, muscle contraction in the form of low-intensity low-amplitude physical activity increased muscle LPL production by 10-fold. Many of the lipid benefits of exercise (improved HDL cholesterol and particle size) may be mediated by the same mechanism. The implications of this may be far-reaching. For example, since LPL insufficiency is associated with abnormalities in blood lipoproteins, and abnormalities in blood lipoproteins are associated with abnormal hormone levels (eg. Low testosterone, etc.), a lack of LPL may contribute to hormone imbalance. Can regular muscle contraction and the avoidance of prolonged sitting naturally improve hormone levels? Hopefully the research on this will continue and inform us more clearly in the future.
Interleukin (IL)-6: In response to muscle contractions, muscle cells release IL-6 both locally in the muscle and into the circulation. In the muscle, IL-6 appears to improve glucose uptake and fat oxidation. At the same time, it may travel through the blood to the liver to increase glucose synthesis and to the fat cells to increase lipolysis (fat break down). This is a nice little system here; through IL-6, the muscle enables itself to better utilize glucose and fat while it simultaneously improves the availability of these fuels in the blood. Through this mechanism, muscle contraction may lower blood glucose and help reduce body fat, from which a number of positive physiological changes follow. Additionally, IL-6 may be responsible for the anti-inflammatory cascade seen as a result of exercise. This suggests that muscle contraction in the form of low-intensity low-amplitude movement throughout the workday, might have a chronic anti-inflammatory effect as well.
IL-15: Less is known about this myokine. IL-15 appears to play a role in muscle growth and lipid metabolism, possibly affecting cardiovascular disease risk. Additionally, a mouse study found that elevated circulating levels of IL-15 resulted in significant reductions in body fat and increased bone mineral content!
Brain Derived Neurotrophic Factor (BDNF): BDNF was named based on its ability to stimulate the growth of new brain cells. However, like many hormone-like compounds, it is produced by, and has effects on, many tissues in the body, including those outside of the brain. Muscle cells appear to produce BDNF, but researchers are not sure that significant amounts are released into the circulation. Within the muscle, it appears to increase fat oxidation and, thus, helps with muscle energy production. If a significant amount of muscle BDNF is actually released into the circulation, it may help reduce the risk of several disorders including Alzheimer's disease, major depression, impaired cognitive function, cardiovascular disease, and type 2 diabetes, and obesity! More research is needed!
Erythropoetin (EPO): This hormone, now infamous due to its use in sports doping, is known mostly for its ability to stimulate the production of red blood cells. Traditional physiology teaches that this hormone is secreted from the kidneys in response to hypoxemia (limited oxygen in the blood) or ischemia (limited blood flow). Both conditions can be generated through exercise, and hypoxemia occurs at high altitude as well. However, it appears that EPO may have additional effects on the body beyond red blood cell production and may be produced by tissues other than the kidneys. While the evidence is not conclusive, it appears that contracting muscle cells may produce and secrete EPO. This muscle derived EPO may then have significant effects on body fat, lean muscle mass, insulin sensitivity, and muscle vascularization. In one study, a gene which enhances EPO production was inserted into a leg muscle in mice. The increase in EPO from that single leg muscle had effects on the entire body, including a 28% reduction in total body fat, a 14% increase in total muscle mass, and a 25% increase in vascularization of the "transfected" muscle. Muscle fat oxidation was increased and insulin levels were normalized as well. While there has been limited research on whether low amplitude, low intensity muscle contraction increases circulating levels of EPO, it remains a very real possibility, making EPO a potentially powerful myokine of movement.
Mitochondria: Mitochondria are the source of cellular energy, and cellular energy is the source of body energy and life itself! Declines and dysfunction in these energy generating cellular compartments may underlie a number of diseases, including Alzheimer's disease, diabetes, chronic fatigue syndrome and fibromyalgia, and various cancers. In contrast, higher mitochondrial numbers and excellent mitochondrial function are associated with reduced disease risk, improved energy and vitality, and greater aerobic capacity. While mitochondria are very different than myokines, they have one very important thing in common; that is muscle contraction. A cascade of events that increases the number of mitochondria (
mitochondrial biogenesis) in a cell is triggered by calcium ion flux and, in short, calcium ion flux occurs with muscle contraction
[30]. Thus, muscle contraction alone can stimulate mitochondria to expand and proliferate. Muscle inactivity, on the other hand, is associated with a reduction in key mitochondrial metabolic proteins as well as a reduction in the replication of mitochondrial DNA and mitochondrial proliferation
[31],
[32]. There is intense interest in nutraceutical, herbal, and pharmaceutical interventions which can increase mitochondria number and function, but let's not forget about movement, the most cost-effective intervention!
Grehlin and Leptin: These two hormones are central to the regulation of food energy intake and metabolism. Grehlin promotes hunger and caloric intake, while leptin promotes satiety (fullness) and fat metabolism.
Grehlin should rise during fasted states (like before a meal) while leptin should rise during fed states (like after a meal). However, one study showed that sitting (compared to standing) resulted in greater hunger and less fullness despite identical food energy intake. Interestingly, the mechanism was different between genders, with sitting males showing higher levels of grehlin compared to standing males, and sitting females showing lower levels of leptin compared to standing females. One likely outcome of increased hunger is excess caloric intake and weight gain over time. Indeed, another study demonstrated that office workers who had more frequent interruptions in sitting time had significantly lower waist circumference than other workers with fewer interruptions. In addition to the grehlin and leptin effects of frequent movement and interruption in sitting time, weight loss and leanness may be promoted simply from increased energy expenditure. A study comparing the energy expenditure of office workers while sitting at a traditional desk vs. walking very slowly at a treadmill desk showed that the walking desk required 119 more calories per hour. Therefore, an overweight person could lose 1 pound per week (3500 calories), or around 45-50 pounds per year, by using a treadmill desk for 6 hours per day during the weekdays. Yet, treadmill desks are not the only option. Another study showed that simply standing at a computer instead of sitting increased caloric expenditure by 81.6 calories per hour. That amounts to almost ¾ of a pound per week of weight loss or 30 to 35 pounds of weight loss per year, with 6 hours of standing per day during the weekdays. However, considering the above discussion about myokines and muscle contraction, our goal will be not simply to stand instead of sit, but to maximize muscle contraction while still effectively working. Hopefully you are already convinced that muscle contraction is the key to avoiding the harms of physical inactivity but, before we talk about how to contract muscles at work, there are a few more very important benefits of muscle contraction that I want to mention.
Don't Just Sit (or Stand) There, Move Something!
In addition the role muscle contraction plays in the optimal function of the endocrine system and human physiology in general, the mechanical forces from muscles contracting in the setting of gravity provide numerous direct benefits as well. For example, the articular cartilage in the joints and intervertebral discs in the spine require these mechanical forces for nourishment and waste product removal. These tissues have no direct blood supply and rely on the "milking" or "pumping" action of movement for health. Without movement, these tissues desiccate (dry) and degenerate (crack and thin), resulting in osteoarthritis and degenerative disc disease. Many are surprised to realize that movement prevents arthritis rather than contributes to it.











.jpg)
.jpg)
.jpg)